Bring the Innovation of Diaton Tonometer to Your Practice GET A QUOTE NOW
Dial Team Diaton at: 1-877-DIATONS
We’re Open and here to assist You
☏ 1-877-342-8667
Bring the Innovation of Diaton Tonometer to Your Practice GET A QUOTE NOW
Dial Team Diaton at: 1-877-DIATONS
The Diaton Tonometer revolutionizes intraocular pressure (IOP) measurement with its pain-free, non-invasive, user-friendly design, providing accurate readings in both clinical and mobile settings.
Non-Invasive & Safe
Measures IOP through eyelid and sclera, reducing infection risk by avoiding corneal contact.
Consistent Accuracy
Delivers reliable IOP readings unaffected by corneal thickness, curvature, scarring, or prior surgeries (LASIK, PRK).
Painless & Hassle-Free
No air puffs, no numbing drops, no sterilization needed. Quick, comfortable, and ideal for children, seniors, and sensitive eyes.
Compatible with Contact & Scleral Lenses
Unlike traditional tonometers, Diaton does not require lens removal, improving patient convenience and accuracy.
Portable & Ready to Use
Lightweight, pre-calibrated, and requires no disposable covers or drops, making it cost-effective and eco-friendly.
Flexible Patient Positioning
Measures IOP in sitting or supine positions, perfect for bedridden patients and emergency use.
Designed for Efficiency & Safety
Supports safety and social distancing protocols by eliminating close patient proximity during IOP measurement.
The Diaton Tonometer is a versatile, innovative tool designed for healthcare professionals and clinical settings where traditional corneal tonometry is challenging or not feasible.
Ophthalmologists & Optometrists
Used for routine eye exams, glaucoma screening, and patient-friendly IOP measurement.
Ophthalmic Technicians
Easy to use with minimal training, enhancing clinical efficiency.
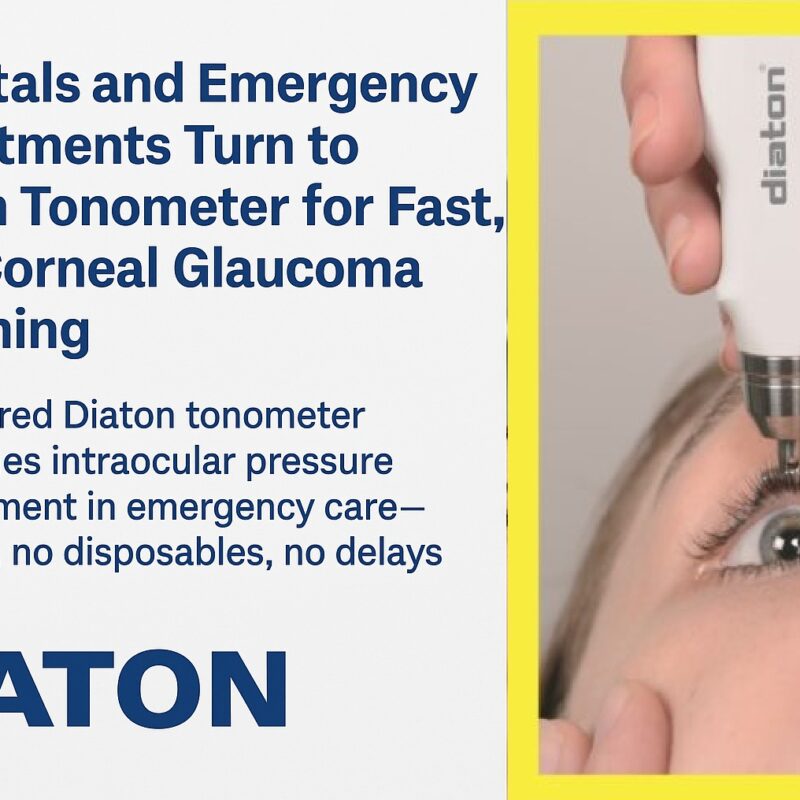
Hospitals & Emergency Departments (ER, ED, Urgent Care)
Provides a quick, non-invasive IOP measurement for critical care.
Nursing Homes & Elder Care Facilities
Enables IOP measurement for immobile or elderly patients with ease.
General & Specialty Practitioners
Useful for basic eye exams and glaucoma screening in various patient demographics.
Medical Missions & Mass Glaucoma Screening
Portable and ideal for large-scale screenings without corneal contact or need for numbing drops.
The Diaton Tonometer excels in situations where corneal tonometry is not ideal or contraindicated, including:
Pediatric Patients
Minimizes discomfort and fear associated with eye exams.
Corneal Pathologies
Works effectively with edema, infections, or post-surgical conditions where corneal contact is unsafe.
Keratoconus & KPro Patients
Ensures accurate measurements despite corneal irregularities.
Eye Trauma Cases
Allows safe IOP assessment without worsening injuries.
Unlike Goldmann applanation or non-contact tonometry, which can be affected by corneal thickness, rigidity, curvature, scarring, and prior surgeries, Diaton’s transpalpebral method ensures accurate readings in diverse patient conditions.
Diaton Tonometer transforms eye pressure measurement with superior safety, precision, and convenience. Learn how Diaton can enhance your practice today!
Interview: Young OD’s of America on Safe Tonometry Solution with CEO of Diaton Tonometer
IN THE VIDEO: Will To, OD aka @thetravelingOD San Mateo, CA Justin Bazan, OD Brooklyn, NY Kirk Kaupke, OD in New York City (NYC) John Nguyen, OD with practices in Bronx, Brooklyn and Staten Island, Roman Iospa, CEO of Diaton Tonometer at DevelopAll Inc, New York
“Diaton tonometry” is a unique approach to measuring intraocular pressure (IOP) through the Eyelid and Sclera. Non-Contact (no contact with cornea), no anesthesia or sterilization required, pen like, hand-held, portable tonometer.
Emil W. Chynn, MD, FASC from Park Avenue LASEK stated, – “As a Cornea-Refractive trained specialist, I encounter many situations where Goldmann readings are inherently inaccurate–like post-LASIK, in cases of corneal edema, scarring, keratoconus, post-keratoprosthesis or transplant. In such cases, it’s both invaluable and reassuring to have the Diaton device available to measure IOP that’s independent of corneal pathology”
“It works,” said Dr. Mark Latina, glaucoma specialist (Harvard / MEEI) and the inventor of Selective Laser Trabeculoplasty (SLT), after revealing results of the study titled: “Accuracy of Transpalpebral Tonometer Diaton Compared to Goldmann Applanation Tonometer in Normal and Glaucomatous Eyes”. “The Diaton device provides a very useful way to confirm Goldmann tonometry, especially in certain complicated patients, in my glaucoma referral practice.”
Henry D. Perry, MD (Corneal Specialist and Comprehensive Ophthalmology – OCLI), – “Transpalpebral Tonometry is an accurate method of IOP measurement that is also independent from the biomechanical characteristics of cornea. It can be recommended for IOP measurements of patients diagnosed with glaucoma including those cases where cornea pathology or cornea characteristics have been altered.”
“The [device] is easy to use, user friendly, and it can be used on patients for mass screening,” Dr. Shazly said. “It’s portable, it’s economical; it’s really good for screening purposes.”
John Hope, MD, an ophthalmologist in private practice in Oklahoma City, said that he prefers the device because applanation tonometry is time-consuming and often requires support staff. Dr. Hope said that he has used the instrument routinely on every patient for at least 6 months.
“This instrument is so user friendly . . . there are no rubber covers to deal with, and, after the initial purchase, it is virtually maintenance-free,” he said.“I clean the instrument with an alcohol pad after each use, and it is easily portable in your pocket and can be transported from room to room or office to office.”
“There is no corneal contact and pressures can be obtained in patients wearing contact lenses,” Dr. Hope concluded. “The technique is easily and quickly learned.”
Dr. Blumenthal, Emergency Department Physician:
“In the fast-paced emergency setting, accurately measuring intraocular pressure (IOP) can be challenging, especially in patients with eye trauma, corneal injuries, or post-surgical conditions. The Diaton Tonometer has been a game-changer, allowing for quick, non-invasive IOP measurements through the eyelid without corneal contact or numbing drops.
It’s fast, reliable, and easy to use, making it an essential tool for glaucoma emergencies and trauma cases. I highly recommend Diaton for any emergency department looking for a safer, more efficient alternative to traditional tonometry.”